Now Accepting Medicaid At All Locations!
Now Accepting Medicaid At All Locations!

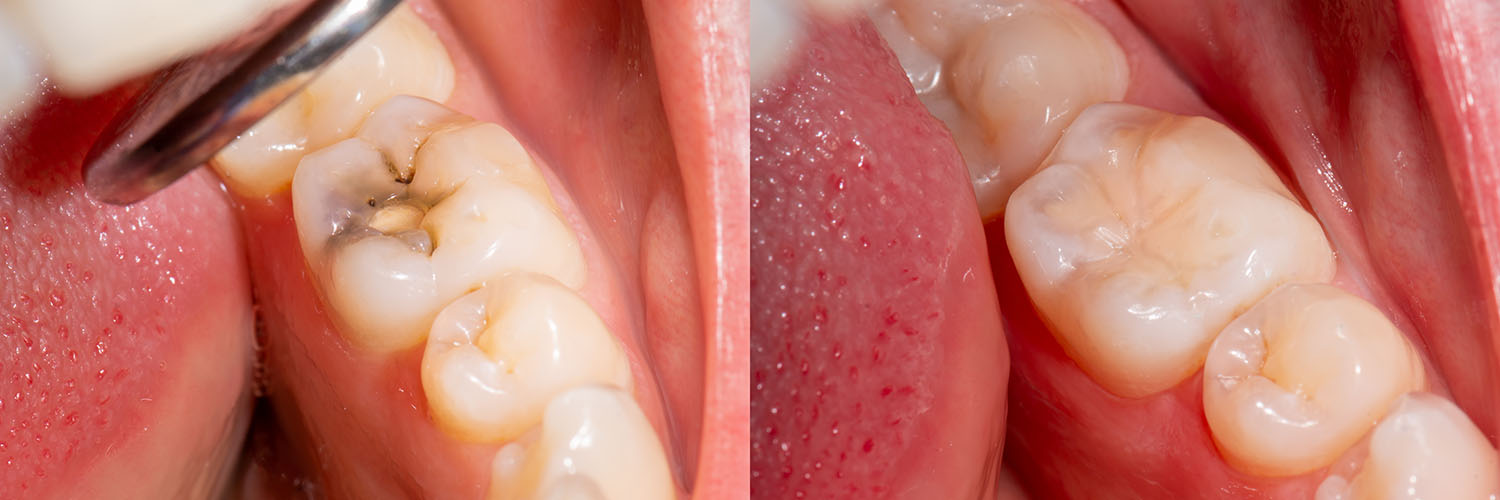
When a tooth is weakened by decay or minor damage, a carefully placed filling restores its shape, strength, and ability to chew without discomfort. Fillings are one of the most common restorative procedures in general dentistry because they stop the spread of decay and preserve healthy tooth structure before more extensive treatment becomes necessary.
Tooth decay remains widespread across age groups, and addressing cavities early helps prevent infection, sensitivity, and the need for more complex procedures. A well-matched filling not only repairs function but also contributes to a natural-looking smile — an outcome that matters to patients who want durable results that blend with their teeth.
Our approach focuses on precise preparation, modern materials, and patient comfort. At New Day Dentistry we emphasize conservative techniques that preserve as much healthy tooth as possible while delivering a restoration that fits, functions, and looks like the original tooth.
Attempts to restore damaged teeth date back millennia, but modern dentistry has refined the science and materials dramatically. Over the last century, practitioners have moved from metal-only restorations to a palette of tooth-colored and biocompatible options that prioritize aesthetics and tissue health alongside strength.
Today’s filling materials offer more predictable bonding to tooth structure and better resistance to wear and staining. That progress means clinicians can often place restorations that are less invasive, more comfortable for patients, and longer lasting than earlier generations of materials.

Selecting the right filling material is a clinical choice guided by the cavity’s size and location, the patient’s bite and oral habits, cosmetic expectations, and the desire to conserve natural tooth. No single material is ideal for every situation, so dentists weigh the trade-offs of strength, longevity, and appearance when recommending an option.
Small to moderate cavities in the visible front teeth often benefit from tooth-colored materials that blend seamlessly with enamel. Conversely, restorations in back molars — where chewing forces are highest — may prioritize durability while still maintaining acceptable esthetics for the patient.
We’ll discuss options and the reasoning behind a recommendation so you can make an informed decision that balances appearance, function, and long-term health for the tooth.
Composite resins are a blend of durable polymers and fine glass or ceramic fillers, available in multiple shades to closely match natural enamel. They are placed directly into the prepared cavity and bonded to the tooth, allowing for a conservative preparation that preserves more healthy structure.
Because composite bonds to enamel and dentin, it can strengthen a compromised tooth and restore its contour without extensive removal of sound tissue. Composites are versatile — they can fill cavities, repair chips, and reshape minor cosmetic flaws — though they can be more susceptible than ceramics to staining over many years.
Amalgam has a long history of reliable service, offering notable durability in high‑stress chewing areas. While it does not match tooth color, amalgam can be an appropriate choice when strength and longevity are the primary concerns, particularly for large back-tooth restorations.
Glass ionomers bond chemically to tooth structure and slowly release fluoride, which can help reduce the risk of recurrent decay at restoration margins. Their ease of use and fluoride release make them valuable in specific clinical situations, such as pediatric care or for restorations near the gumline.
Because glass ionomers are generally less wear‑resistant than composites or ceramics, they are often used where forces are light or as a temporary or transitional restoration.
Ceramic restorations are fabricated from dental porcelain and designed outside the mouth, then cemented or bonded into place. They offer excellent color matching, high resistance to staining, and robust wear characteristics, making them an excellent long‑term option for larger cavities that require an indirect restoration.
Because they are custom‑made, ceramics combine strength and esthetics but typically require two visits: one to prepare and capture impressions and another to place the finished piece.
Metal restorations, including gold alloys, remain a durable and biocompatible choice for some patients. Gold is gentle to opposing teeth and resists corrosion, but its metallic appearance and higher material cost have made it less common for visible areas of the mouth.
When a cavity is identified, the treatment plan begins with a careful evaluation of the tooth’s condition, the extent of decay, and any symptoms the patient may have. Radiographs and visual inspection help determine whether a simple filling is appropriate or if a more extensive restoration will be necessary.
The procedure itself is typically efficient and designed for patient comfort. After administering local anesthetic as needed, the dentist gently removes decayed tissue and shapes the remaining tooth to receive the chosen restorative material. Modern tools — including high-speed instruments, air abrasion, or lasers in certain cases — allow precise removal while protecting healthy structure.
Once the cavity is prepared, the selected material is placed using techniques specific to that material: composites are layered and cured with a light, glass ionomers are set to bond chemically, and indirect restorations are cemented during a follow-up appointment. Before you leave, your bite will be checked and adjustments made so the restoration feels natural while chewing.
Proper care following a filling helps ensure it performs well for years. Immediately after treatment, you may notice numbness from anesthesia or mild sensitivity to temperature; both are common and usually resolve within days to weeks. If sensitivity persists or increases, your dental team should evaluate the tooth to rule out other causes.
Good daily habits — brushing twice, flossing daily, and attending routine dental checkups — preserve restorations and the teeth around them. Avoiding hard, brittle foods and taking care with habits such as opening packages with teeth or chewing on ice reduces the risk of chipping or dislodging a filling.
Regular follow-up exams allow your dentist to monitor restorations for wear, marginal breakdown, or recurrent decay. When concerns are identified early, repairs or replacement can be planned before a small problem becomes a larger one.
Temporary numbness
You may have reduced sensation for an hour or two after local anesthetic. Until feeling returns, avoid chewing on the treated side to prevent accidental biting of soft tissues.
Minor adjustment period
A new filling can feel a little unfamiliar at first. If your bite feels high or you notice persistent discomfort when biting, contact the office so your dentist can fine‑tune the restoration.
Short-term sensitivity
Some temperature or pressure sensitivity is normal after a restoration and typically subsides on its own. If you experience increasing pain, swelling, or any other concerning symptoms, arrange an evaluation.
Long-term maintenance
With daily oral hygiene and periodic professional care, most restorations deliver many years of reliable service. Proper technique and attention to risk factors like bruxism or high sugar intake help extend the life of a filling.
We aim to make each restorative visit as clear and comfortable as possible. If you have questions about your procedure, materials, or any follow-up needs, please reach out to our office for guidance.

Dental fillings are a straightforward, effective way to halt decay, restore tooth function, and maintain the appearance of your smile. Advances in materials and placement techniques allow dentists to deliver solutions that are both strong and natural-looking while preserving healthy tooth tissue whenever possible.
If you’re concerned about a sensitive tooth, visible dark spots, or any change in how a tooth feels, early evaluation makes the best outcome more likely. Our team can explain material options, the treatment process, and what to expect during recovery.
For more information about fillings or to discuss treatment for a specific tooth, please contact us; we’ll be happy to help you understand your options and schedule an appointment if needed.
Dental fillings are restorations placed into teeth after decay or minor damage has been removed to restore shape, strength and normal chewing function. They stop the progression of cavities by sealing the defect and protecting the inner tooth from bacteria and sensitivity. By addressing decay early, fillings help avoid more invasive procedures and preserve natural tooth structure.
A well-placed filling also contributes to a natural-looking smile by matching the tooth’s form and, when possible, its color. Modern techniques focus on conservative removal of decayed tissue so more healthy tooth remains intact. Your dentist will explain which restoration best balances longevity, function and appearance for your specific tooth.
Determining the need for a filling begins with a thorough clinical exam and often includes radiographs to reveal decay between teeth or below the enamel surface. Dentists evaluate the extent of decay, any symptoms such as pain or sensitivity, and the tooth’s structural integrity to decide whether a simple filling will suffice. The decision takes into account the patient’s overall oral health and risk factors that could accelerate decay.
Symptoms like lingering sensitivity to hot or cold, a visible dark spot, or discomfort when biting can prompt an evaluation even if routine X-rays are not yet showing extensive damage. Early detection allows for more conservative treatment and better long-term outcomes. Your clinician will discuss findings and recommended next steps so you understand the reasoning behind a proposed restoration.
Several common materials are used for fillings, each with distinct properties: composite resins are tooth-colored and bond to enamel and dentin, amalgam provides durable service in high-stress chewing areas, glass ionomer cements offer fluoride release and chemical bonding, and ceramic or gold restorations deliver excellent longevity for larger defects. Material choice depends on the cavity’s size and location, aesthetic goals, and the functional demands placed on the tooth. At New Day Dentistry we review the advantages and limitations of each option so patients can make informed decisions.
Composites are chosen when appearance and conservation of tooth structure are priorities, while amalgam or metal-based options may be selected when maximum wear resistance is required. Glass ionomers are useful for certain pediatric situations or where fluoride release is helpful, and indirect ceramics or gold are reserved for larger restorations that benefit from lab fabrication. Your dentist will recommend the material that best balances strength, appearance and long-term health for the tooth in question.
The filling appointment typically begins with a review of the diagnosis and application of local anesthetic when needed to ensure comfort throughout the procedure. The dentist removes decay using precise instruments and prepares the cavity to receive the chosen material while preserving as much healthy tooth structure as possible. Modern techniques and tools allow efficient, controlled treatment with minimal discomfort for most patients.
Placement varies by material: composites are applied in layers and cured with a light, glass ionomers set chemically, and indirect restorations such as inlays are cemented at a follow-up visit. The dentist will check and adjust your bite before you leave so the restoration feels natural during chewing. If you have concerns about anxiety or comfort, discuss available options with the team before treatment.
Immediately after treatment you may notice numbness from the anesthetic or mild sensitivity to temperature and pressure; these effects usually resolve within days to a few weeks. Until feeling returns, avoid chewing on the treated side to reduce the chance of biting soft tissues accidentally and to allow the restoration to settle. If you experience increasing pain, swelling or persistent sensitivity, contact your dental team for an evaluation.
Long-term care for a filling includes brushing twice daily with fluoride toothpaste, flossing daily and attending regular dental checkups to monitor the restoration for wear or marginal breakdown. Avoid using teeth as tools and be cautious with very hard or sticky foods that can chip or dislodge a filling. Regular professional cleanings and timely attention to any changes help preserve the life of the restoration and surrounding tooth structure.
The lifespan of a filling varies with the material used, the size and location of the restoration, and the patient’s oral habits and hygiene. Smaller composite restorations in low-stress areas may last many years, while larger restorations in back teeth or patients who grind their teeth may experience earlier wear. Proper home care and routine dental visits allow your dentist to spot early signs of wear or recurrent decay and address them before failure occurs.
Other factors that influence longevity include diet, oral bacteria levels, and any existing dental conditions such as bruxism (teeth grinding). Regular monitoring enables timely repair of minor issues, which can extend a restoration’s useful life. If a filling shows breakdown, replacement or an alternative restoration can be planned to restore function and protect the tooth.
Tooth-colored composite resins are widely used because they bond to tooth structure, can be shaded to match enamel, and allow conservative preparations that preserve healthy tissue. They are an excellent choice for front teeth where appearance is a priority and for many posterior restorations when properly placed and maintained. Composites also help support weakened teeth by bonding to dentin and enamel, which can reduce the need for more extensive restorations.
Limitations include a greater susceptibility to staining over many years and potentially higher wear in extremely high-load situations compared with some ceramics or metal-based materials. For very large cavities or when chewing forces are unusually high, your dentist may recommend an indirect restoration such as an onlay or crown. Discussing your functional needs and cosmetic goals with your clinician will help determine the best material for each tooth.
Inlays, onlays and crowns are indirect restorations used when a cavity or structural loss is too extensive for a direct filling to provide reliable strength and longevity. These restorations are fabricated outside the mouth, often in ceramic or metal alloys, and are chosen when the remaining tooth needs reinforcement or when a precise fit and superior wear resistance are desired. They are especially useful for large posterior defects where a direct filling would risk fracture or marginal breakdown.
The process typically involves preparing the tooth, taking an impression or digital scan, and placing a temporary restoration until the final piece is fabricated and cemented at a second appointment. Indirect restorations can restore more tooth structure and distribute chewing forces more evenly, which often improves long-term outcomes for heavily restored teeth. Your dentist will evaluate whether a direct or indirect approach best preserves function and reduces future risk.
If a cavity is left untreated, decay can progress deeper into the tooth toward the pulp where nerves and blood vessels reside, leading to increased sensitivity, persistent pain and infection. Advanced decay may require root canal treatment to remove infected tissue, or in severe cases the tooth may become nonrestorable and require extraction. Infection can also spread to adjacent tissues and, if unchecked, contribute to broader health concerns that warrant prompt attention.
Early treatment of cavities is less invasive and more likely to preserve natural tooth structure, reducing the need for complex restorative or surgical procedures. Regular dental exams and timely intervention when decay is detected are the most effective ways to prevent progression. If you notice changes such as pain, swelling or a new dark spot on a tooth, schedule an evaluation to address the issue before it worsens.
The practice emphasizes conservative techniques, careful diagnosis and modern materials that allow removal of only diseased tooth tissue while maintaining as much healthy structure as possible. Clinicians use targeted local anesthetic, advanced instrumentation and adhesive bonding methods that reduce the need for extensive mechanical removal. These approaches help restore function and appearance with minimal discomfort and faster recovery for patients.
Communication and patient comfort are also central to care; the dental team explains options, expected sensations and follow-up needs so patients know what to expect before treatment begins. Digital imaging and precise preparation protocols help ensure accurate restorations and predictable outcomes. At New Day Dentistry we combine clinical experience with contemporary technology to deliver restorations that protect long-term oral health and patient well-being.